Javier Segovia Cubero1, Nicolás Manito Lorite2 1Unit of Advanced Heart Failure and Heart Transplantation, Service of Cardiology, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain. 2Unit of Heart Failure and Heart Transplantation, Hospital Universitario de Bellvitge, L’Hospitalet de Llobregat, Barcelona, Spain. Corresponding author: Javier Segovia…
Javier Segovia Cubero1, Nicolás Manito Lorite2
1Unit of Advanced Heart Failure and Heart Transplantation, Service of Cardiology, Hospital Universitario Puerta de Hierro, Majadahonda, Madrid, Spain.
2Unit of Heart Failure and Heart Transplantation, Hospital Universitario de Bellvitge, L’Hospitalet de Llobregat, Barcelona, Spain.
Corresponding author: Javier Segovia Cubero, MD, PhD, Service of Cardiology, Hospital Universitario Puerta de Hierro, C/ Manuel de Falla 1, E-28222 Majadahonda, Madrid, Spain. E-mail: [email protected]
Abstract (word count 197)
Aims: This study aimed to gather information of the opinion of cardiologists regarding different aspects related to adherence to medication of patients with heart failure.
Methods and results: A total of 158 cardiologists (mean age 44 years) participated in a qualitative, cross-sectional and multicenter survey study, and complete a 29-item questionnaire. The mean years of practice was 18 (9.4) years. Clinical criteria (Framingham) were the preferred option to establish the diagnosis by 58.3% of respondents, and improvement of prognosis the preferred option for treatment decisions by 80%. The use of active criteria for the search of adherence was stated by 80% of participants, and the lack of time the main reason for not establishing these criteria. Patient’s education was a major contributor to adherence, and having available an established plan of prescribed medication was rated as very influential to improve adherence. Good doctor-patient communication was considered by 82% as one of the most important modifiable factor, as well as joining two or more active principles in a single pill (98% of participants).
Conclusions: This survey study provides useful information regarding the opinion of cardiologists regarding relevant aspects of treatment adherence in HF patients treated in daily practice.
Keywords: Heart failure; medication adherence; survey study.
Introduction
Heart failure (HF) remains a major health care problem and is the leading cause of hospitalization in people older than age 65 in US and Europe, accounting for 1-2% of all admissions [1,2]. In a recent study of temporal trends of HF in a representative sample of the UK population between 2002 and 2014, a 12% increase in the estimated newly diagnosed cases and a 23% increase in the absolute number of cases was found [3]. This was accompanied by an increase in patient age and multi-morbidity at first presentation [3]. However, despite significant decline in the age- and sex-adjusted incidence of HF, the overall prevalence and associated total burden of the disease has markedly increased, particularly due to the population growth and increased longevity [4]. In addition, hypertension, ischemic heart disease, diabetes, obesity, and smoking underlie over half incident HF cases [5]. According to recent statistics jointly published by the American Heart Association and American College of Cardiology, one third of the adult population in the US has stage A HF, defined as the presence of predisposing conditions for HF [6].
Non-adherence with medication and diet has been consistently recognized as an essential precipitating factor leading to decompensations of chronic HF and contributing to hospitalization, poor clinical outcomes and high healthcare costs [7-10]. Medication is a critical part of HF treatment, and adhering to medication regimens is a key behavior in HF self-care. Although medication adherence is a major component of HF self-care behaviors, concurrent treatment of multiple comorbidities adds further complexity to the medication therapy regimens for patients with HF [11]. It has been shown that almost half of patients hospitalized with heart failure need to start at least 1 new medication, 24% having indications for at least 2 medications, and 14% for ≥ 3 medications in order to comply with current guidelines [12]. Rates of adherence reported in HF studies have varied from 10% to 98% depending on the measuring instruments used, and most authors have noted an average of 40-60% of medication adherence [13].
A clear interaction exists between adherence and the subsequent prognosis. In a cohort study, non-adherent patients accounted for 22.1% of all hospital admissions for clinically manifest HF, and they had a markedly shorter time interval until readmission to hospital [14]. Likewise, it is well known that low adherence to antihypertensive medication notably increases the risk for clinically manifest HF [15]. In a comprehensive systematic review of 57 intervention studies designed to assess the effect of adherence to HF medication on clinical outcomes, overall medication adherence interventions significantly reduced mortality risk among HF patients (relative risk [RR] 0.89, 95% confidence interval [CI] 0.81-0.99) and decreased the likelihood of hospital admission (odds ratio [OR] 0.79, 95% CI 0.71-0.89) [16]. Also, different studies have shown that physicians uptake of guideline recommendations that improve HF outcomes remains suboptimal [17-20].
Despite the increasing awareness of the need for assessing medication adherence in HF patients in daily practice, only a few studies have investigated factors related to medication adherence in Spain [21,22]. Therefore, a survey study was designed, the primary objective of which was to gather information on the opinion of specialists regarding different pharmacological and non-pharmacological aspects related to medication adherence in patients with HF attended in the real-world setting. Knowledge of the current situation is an indispensable step to develop adequate strategies to improve medication adherence in HF patients.
Methods
Study design
This was a health system research cross-sectional, multicenter and non-randomized study (The METRICA Study), which was carried out in the framework of outpatient clinics of Cardiology of public and private centers throughout Spain. METRICA is the Spanish acronym of MEjor EsTRategia para incrementar la adherencia al tratamiento de la Insuficiencia CArdiaca (Best Strategy to Improve Adherence to Treatment in Heart Failure). The study was carried out over a period of 2 months, from April 1 to May 31, 2018. The study protocol was approved by the Ethical Committee for Clinical Research of Hospital Clínico Universitario San Carlos, Madrid, Spain.
The general purpose of the study was to make a first approach to the actual situation of adherence to current recommendations and treatments in the management of the patient with HF in Spain. The primary objective of the study was to assess factors affecting adherence to treatment of HF patients. The secondary objective was to propose the first actions to be carried out to improve adherence to treatment of the patient with HF.
Participants and procedures
The study questionnaire was developed by a scientific committee appointed specifically for the development and implementation of the project. Three study coordinators who were members of the scientific committee (J.S.C, N.M.L, R.B.F.) participated in the development of the protocol and supervised the progression of the study, including recruitment of participants and results of data analysis.
The final questionnaire was composed of 29 items and was divided into five sections: section 1 included 4 items with questions regarding management of HF; section 2 included 6 items with questions related to adherence to treatment; section 3 included 7 items related to non-modifiable factors associated to adherence; section 4 included 9 items related to modifiable factors associated with adherence, and section 5 included 3 items related to actions to be performed to improve adherence to treatment in HF patients. In addition, general data related to demographic characteristics of participants, type of practice, participation in research projects and training programs focused on HF, and membership of scientific societies were recorded. The study questionnaire is described in the Supplementary Material.
Candidates to participate in the study were cardiologists involved in the care of patients with HF attended in public or private consultations throughout Spain. Cardiologists were eligible, provided that they usually take care of a minimum of 10 patients with HF on a monthly basis. Cardiologists who attended less than 10 patients with HF on a monthly basis were excluded.
The participants were recruited through invitations sent by e-mail to cardiologists registered in the Medynet database, the first Internet node exclusively devoted to the health care sector in Spain that currently includes data of approximately 190,000 users (http://cme.medynet.com/). The sample was non-randomized stratified by non-proportional affixation to the number of physicians by strata in the autonomous communities. Participation in the study was anonymous, and voluntary. The study questionnaire was lodged in an Internet microsite to which participants accessed via a weblink included in the e-mail. Physicians who met the inclusion criteria and accepted to participate in the study were provided with the microsite URL and the user’s password.
Statistical analysis
With a sample size of 150 participants, a margin error of approximately 5% is obtained for a confidence level of 95% and with heterogeneity of 50%. Descriptive statistics included frequencies and percentages for categorical variables, and mean and standard deviation (SD) for continuous variables. Data were analyzed using the SAS statistical program (Statistical Analysis Systems, SAS Institute, Cary, NC, USA) version 9.1.3 for Windows.
Results
Participants
A total of 158 cardiologists volunteered to participate in the study. There were 108 men and 50 women, with a mean (standard deviation, SD) age of 44.3 (9.4) years. The mean years of practice was 17.8 (9.4) years. Eighty-three percent of respondents have participated in a training program on HF in the last 12 months, and 46% have participated in a research project on HF. Almost all participants (96%) belonged to a scientific society, with the Spanish Society of Cardiology (SEC) and the European Society of Cardiology (ESC) as the most frequent (93% and 57% of the cases, respectively). Also, 97% of participants worked in the hospital setting (tertiary care hospitals in 57% of cases), with HF units available in 74% of the centers. Eighty-three percent of the 117 cardiologists who worked in a hospital with HF unit, participated in the activities of that unit.
Management of heart failure
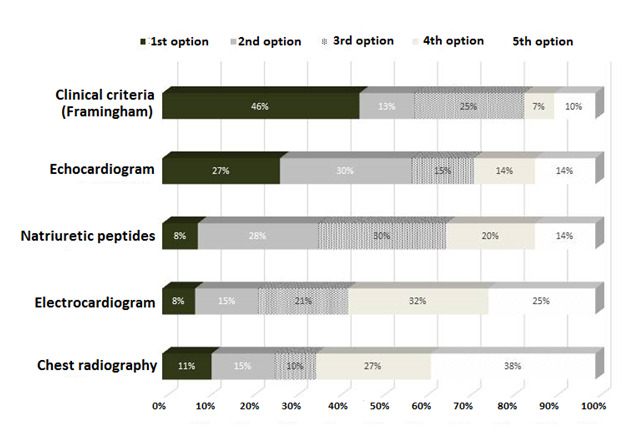
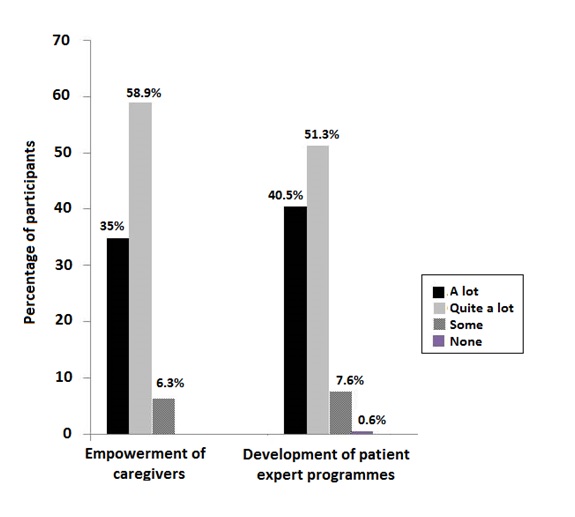
Ninety-three percent of participants stated that they followed the 2016 ESC Guideline on the diagnosis and treatment of acute and chronic HF, 6% followed the ACCF/AHA Guideline for the Management of Heart Failure, and the remaining 1% the NICE guideline “Chronic heart failure in adults: management”. Regarding the options used for the diagnosis of HF (Figure 1), clinical criteria (Framingham) was the preferred choice, and 58.3% of participants selected this item as the first or second option, followed by the echocardiogram selected by 57.6%. By contrast, natriuretic peptides and electrocardiogram were first options selected only by 8% of participants.
Figure 1. Distribution of the percentages of responses regarding the preferred options of cardiologists for the diagnosis of heart failure (HF).
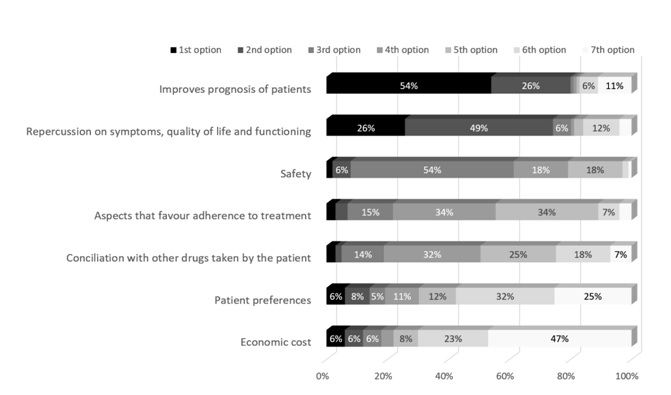
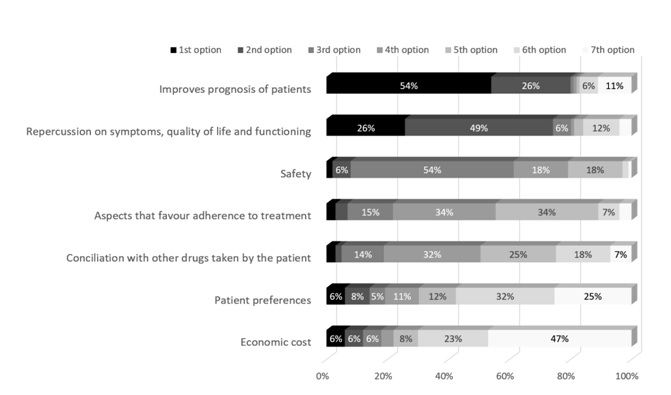
 Factors associated with therapeutic decisions taken by cardiologists in the care of patients with HF are shown in Figure 2. The most frequently selected factor affecting treatment decisions was “improves the prognosis of the patient” (this item was selected as first or second option by 80% of participants) followed by “repercussion on symptoms, quality of life and patient’s functioning capacity” (this item was selected as first or second option by 75% of participants). Only 6% of participants selected “aspects that favour adherence to treatment” as first or second option in their therapeutic decision. Regarding the percentage of HF patients receiving specific treatment in which medication should be changed because of side effects, 65.8% of participants reported medication changes in up to 25% of patients and 30.4% between 26 and 50%.
Figure 2. Distribution of the percentages of responses regarding factors that intervene in the therapeutic decisions in patients with heart failure (HF).
Factors associated with therapeutic decisions taken by cardiologists in the care of patients with HF are shown in Figure 2. The most frequently selected factor affecting treatment decisions was “improves the prognosis of the patient” (this item was selected as first or second option by 80% of participants) followed by “repercussion on symptoms, quality of life and patient’s functioning capacity” (this item was selected as first or second option by 75% of participants). Only 6% of participants selected “aspects that favour adherence to treatment” as first or second option in their therapeutic decision. Regarding the percentage of HF patients receiving specific treatment in which medication should be changed because of side effects, 65.8% of participants reported medication changes in up to 25% of patients and 30.4% between 26 and 50%.
Figure 2. Distribution of the percentages of responses regarding factors that intervene in the therapeutic decisions in patients with heart failure (HF).
 Adherence to treatment
Results of this section of the questionnaire are shown in Table 1. The participants of the study had a median of 518 patients assigned to their consultations. A total of 44.9% of cardiologists stated that between 26% and 50% of patients attended in the last week were diagnosed with HF. Also, 127 participants (80.4%) reported to establish active search criteria for adherence to treatment in their patients, using direct questioning in the majority of cases (81.9%). However, in the remaining 31 participants (19.6%) not assessing adherence to treatment, lack of time was the main reason argued by 77.4% of them.
Adherence to treatment
Results of this section of the questionnaire are shown in Table 1. The participants of the study had a median of 518 patients assigned to their consultations. A total of 44.9% of cardiologists stated that between 26% and 50% of patients attended in the last week were diagnosed with HF. Also, 127 participants (80.4%) reported to establish active search criteria for adherence to treatment in their patients, using direct questioning in the majority of cases (81.9%). However, in the remaining 31 participants (19.6%) not assessing adherence to treatment, lack of time was the main reason argued by 77.4% of them.
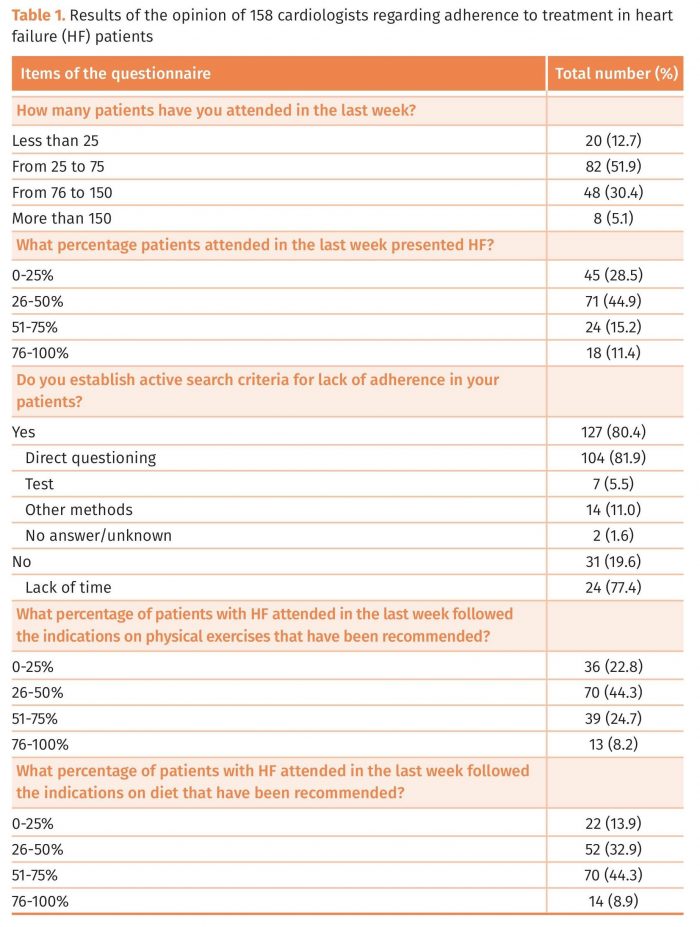 Overall, 67.1% of cardiologists recognized that less than 50% of patients followed recommendation on physical exercise. The percentages of participants who stated that between 0-25%, 26-50%, 51-75% and 76-100% of patients attended in the last week followed their recommendations were 22.8%, 44.3%, 24.7%, and 8.2%, respectively. On the other hand, between 51% and 75% of patients with HF attended in the last week followed recommendations on diet as stated by 44.3% of participants.
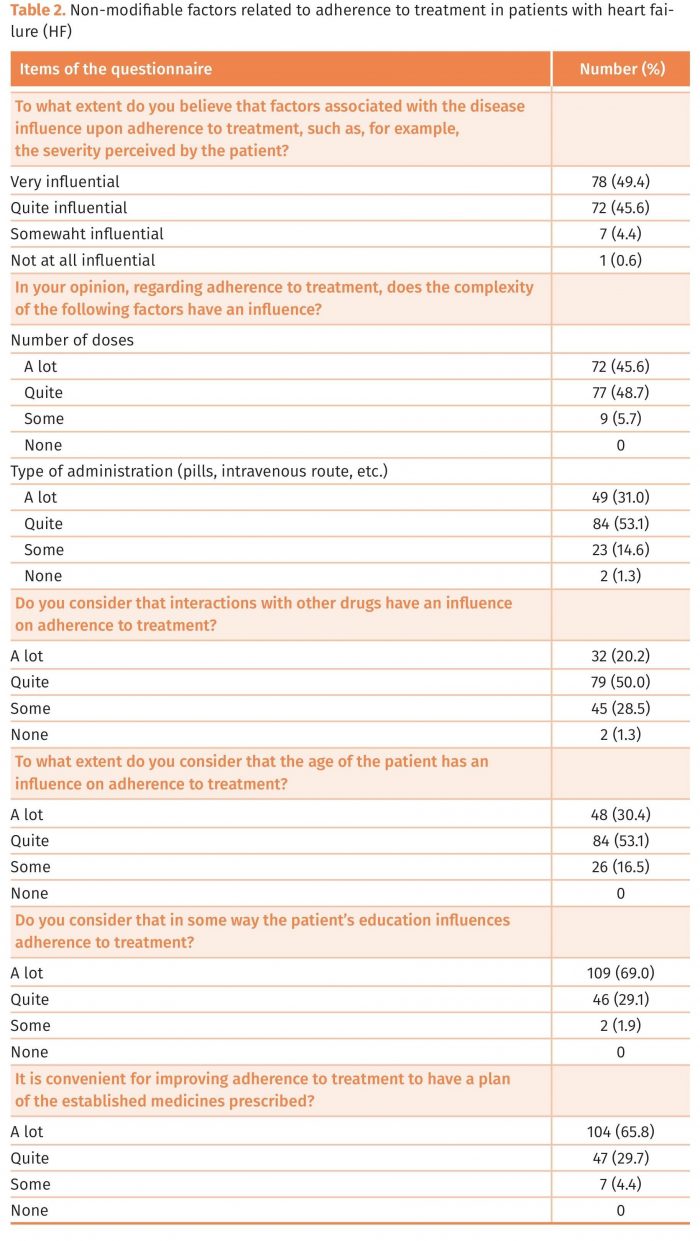
Non-modifiable factors associated with adherence to treatment
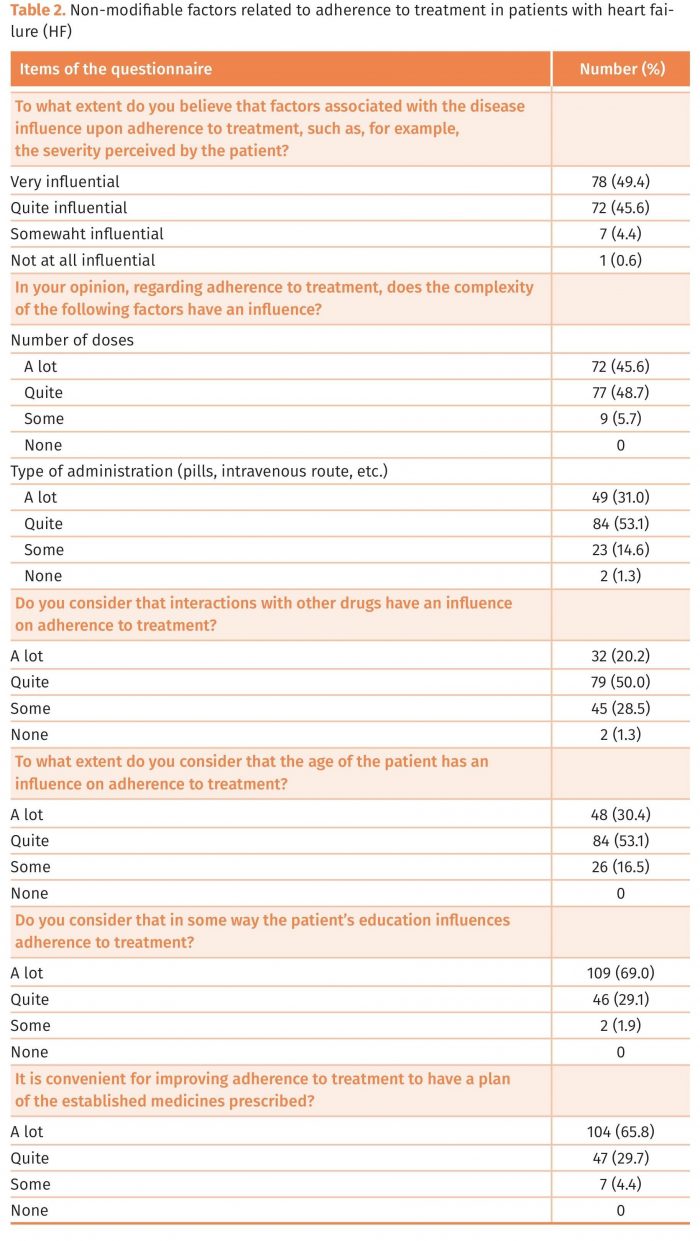
Results of this section of the questionnaire are shown in Table 2. Non-modifiable factors that were rated by participants as having “a lot” influence on adherence included to have an established plan of the prescribed medication (65.8% of respondents), patient’s education (69%), severity of illness perceived by the patient (49.4%), number of doses (45.6%), type of administration (31%), the age of the patient (30.4%), and interactions with other drugs (20.2%). However, almost all participants (98%) considered that the patient’s education influenced “a lot” or “quite a lot” in medication adherence, 95.5% that having available an established plan of prescribed medication influenced “a lot” or “quite a lot”, and 83.5% that the patient’s age influenced “a lot” or “quite a lot” in the adherence to treatment. Also, 91.8% of participants stated that in the chronic stage of the disease there was more risk for non-adherence to treatment.
Overall, 67.1% of cardiologists recognized that less than 50% of patients followed recommendation on physical exercise. The percentages of participants who stated that between 0-25%, 26-50%, 51-75% and 76-100% of patients attended in the last week followed their recommendations were 22.8%, 44.3%, 24.7%, and 8.2%, respectively. On the other hand, between 51% and 75% of patients with HF attended in the last week followed recommendations on diet as stated by 44.3% of participants.
Non-modifiable factors associated with adherence to treatment
Results of this section of the questionnaire are shown in Table 2. Non-modifiable factors that were rated by participants as having “a lot” influence on adherence included to have an established plan of the prescribed medication (65.8% of respondents), patient’s education (69%), severity of illness perceived by the patient (49.4%), number of doses (45.6%), type of administration (31%), the age of the patient (30.4%), and interactions with other drugs (20.2%). However, almost all participants (98%) considered that the patient’s education influenced “a lot” or “quite a lot” in medication adherence, 95.5% that having available an established plan of prescribed medication influenced “a lot” or “quite a lot”, and 83.5% that the patient’s age influenced “a lot” or “quite a lot” in the adherence to treatment. Also, 91.8% of participants stated that in the chronic stage of the disease there was more risk for non-adherence to treatment.
 Modifiable factors associated with adherence to treatment
A large majority of participants (90.5%) completely agree (50%) or quite agree (40.5%) that strategies directed to improve adherence should be established at individual level rather than collectively. As shown in Table 3, items that were considered “very influential” regarding adherence to treatment were a good doctor-patient relationship (stated by 82.3% of participants) and patient’s knowledge of his/her disease (stated by 70.2% of participants). The lack of coordination between different healthcare levels was reported as very influential on adherence by 51.3% of cardiologists. Other modifiable factors that may improve adherence “a lot” were family and social support (stated by 67.1% of participants), strategies based on joining two or more active principles in a single pill (stated by 69.6% of participants), and to have available an established plan of medicines prescribed for the treatment of HF (stated by 53.8% of participants). Specific intervention strategies to improve adherence and patient’s knowledge of the characteristics of their medications were also considered to have “a lot” of influence by 42.4% and 35.4% of participants, respectively.
Modifiable factors associated with adherence to treatment
A large majority of participants (90.5%) completely agree (50%) or quite agree (40.5%) that strategies directed to improve adherence should be established at individual level rather than collectively. As shown in Table 3, items that were considered “very influential” regarding adherence to treatment were a good doctor-patient relationship (stated by 82.3% of participants) and patient’s knowledge of his/her disease (stated by 70.2% of participants). The lack of coordination between different healthcare levels was reported as very influential on adherence by 51.3% of cardiologists. Other modifiable factors that may improve adherence “a lot” were family and social support (stated by 67.1% of participants), strategies based on joining two or more active principles in a single pill (stated by 69.6% of participants), and to have available an established plan of medicines prescribed for the treatment of HF (stated by 53.8% of participants). Specific intervention strategies to improve adherence and patient’s knowledge of the characteristics of their medications were also considered to have “a lot” of influence by 42.4% and 35.4% of participants, respectively.
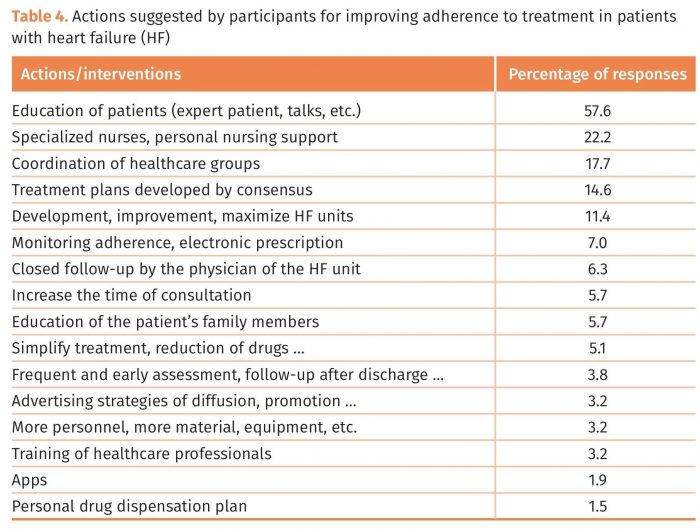
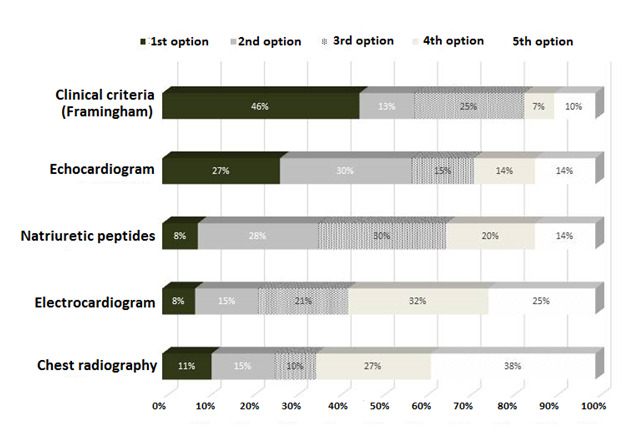
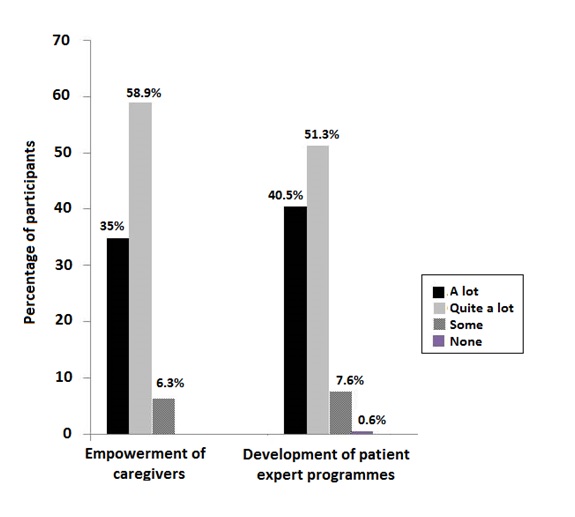
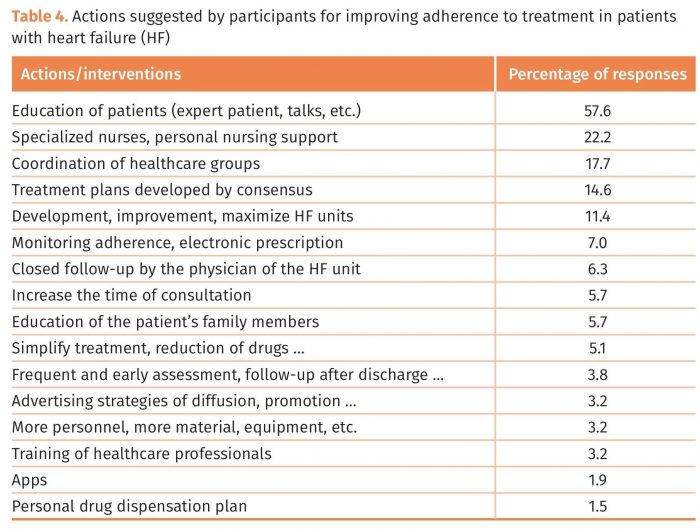
 A total of 93.7% of participants considered that empowerment of caregivers could facilitate “a lot” or “quite a lot” therapeutic adherence. Also, 91.8% of participants believed that expert patient programmes could notably improve adherence (Figure 3). In relation to the open question of actions that may be perform in the cardiologist’s setting to improve adherence are summarized in Table 4, being, patient education-related interventions, involvement of training nurses and coordination of healthcare groups the most frequently stated.
Figure 3. Actions to improve adherence to treatment in heart failure. Percentages of response of participants according to influence on adherence.
A total of 93.7% of participants considered that empowerment of caregivers could facilitate “a lot” or “quite a lot” therapeutic adherence. Also, 91.8% of participants believed that expert patient programmes could notably improve adherence (Figure 3). In relation to the open question of actions that may be perform in the cardiologist’s setting to improve adherence are summarized in Table 4, being, patient education-related interventions, involvement of training nurses and coordination of healthcare groups the most frequently stated.
Figure 3. Actions to improve adherence to treatment in heart failure. Percentages of response of participants according to influence on adherence.
 Discussion
This study provides information on the opinion of cardiologists involved in the care of patients with HF regarding different aspects related to treatment adherence. Despite the decrease of cardiovascular mortality and the introduction of effective and safe medication treatments, HF continues to be a common cause of death and a leading disorder for the need of hospitalization and in-patient care [23]. Moreover, therapeutic recommendations developed in guidelines for the diagnosis and management of acute and chronic HF are applied to an unsatisfactory degree in daily practice [24]. There are multiple factors involved in suboptimal compliance with guidelines, including unawareness of the recommendations, poor acceptance due to discrepancies between guidelines in particular aspects, difficulties of implementation in routine practice related to local circumstances, equivocal assessment of the patient’s risk, or lack of coordination among the different specialists involved in the management of HF patients.
On the other hand, poor adherence has been consistently recognized as an important factor that compromises patient outcomes. Non-compliance is common in elderly patients with HF as were shortcomings in patients’ knowledge regarding prescribed medication, despite efforts to give adequate information [25]. In our study, 84% of participants considered that the patient’s age influences a lot or quite a lot on adherence to treatment. Likewise, it has been shown that forgetfulness, social support, and patient-provider relationship are related to adherence. Providers seeking to increase adherence must consider patients' expectations for their health, their environment, their barriers to following prescribed regimen, and their understanding of their condition and how it relates to medication prescribed [26]. In the present survey, patient’s knowledge of the disease and patient’s knowledge of the medicines prescribed were recognized as important influential factors related to adherence by 95.5% and 83.5% of cardiologists, respectively. In this respect, more than half of participants (57.6%) mentioned patient education as the first action to be implemented in their settings to improve adherence.
Also, good patient-doctor communication was reported as a very influential factor of adherent behaviour. It has been shown that patient-provider interactions appear to be a major determinant of medication adherence [27]. Providing tailored information, patient satisfaction with the communication received, and beliefs about medication are connected and can lead to improved medication adherence. Poor physician communication alone increases the risk of non-adherence. In a meta-analysis of 106 studies assessing the relationship between patient treatment adherence and physician-patient communication, there was a 19% higher risk of non-adherence among patients whose physician communicates poorly than among patients whose physician communicates well [28]. In addition, 95.5% of cardiologists considered that having available an established plan of prescribed medications is a very convenient or quite convenient as a practical tool to improve adherence. The provision of clear written instructions is a well-known method to improve adherence [29]. Mobile applications, automated check-ins, and text message medication reminders have been suggested as potential modes for improving adherence [30].
Some 80% of participants established criteria of active search of lack of adherence in their patients, with direct questioning at the patient interview in 82% of the cases. However, direct questioning may not provide accurate assessments, especially if closed-ended or judgmental questions are posed [31]. In the group of participants that did not use active criteria to examine medication adherence, lack of time was the main reason argued by 77% of participants. In this respect, there is a need for improvement establishing the adequate measures in the organization of the healthcare system at local levels, in order to allow sufficient time during routine consultations. Nurses have a key role in educational interventions, monitoring of decompensation signs, and improve treatment adherence especially in patients with HF followed by the nursing staff in specialized clinics.
Factors related to treatment that showed a higher impact on therapeutic decisions were, firstly, the aim of improving the prognosis of patients with HF and, secondly, the effect of treatment of amelioration of symptoms and improvements of the quality of life and functioning capacity of patients. Preferences of the patient, economic cost, conciliation with other drugs, safety or aspects favouring adherence were not rated as proprieties for treatment decisions, with percentages of participants selecting these reasons as first options ranging between 2% and 6%. In relation to diagnosis of HF, clinical criteria (Framingham) were stated as first or second option by 59% of participants. Echocardiogram was selected as first or second option by 57.1% of cardiologists. This would indicate the need and importance of clinical suspicion of HF before confirmation of diagnosis by echocardiography. In the present survey, questions regarding how patients with HF are managed, in particular, to assess details of their medical treatment were not included, so that whether prescription of recommended medications in daily practice differs from guidelines was not examined. Results of the Euro Heart Failure Survey have shown that the prescription of recommended medications including ACE inhibitors and beta-blockers remains limited and that the daily dosage remains low, particularly for beta-blockers [32]. Recently, a large-scale HF registry in the Netherlands, the CHECK-HF registry, which enrolled nearly 11,000 unselected patients with chronic HF treated in outpatient clinics was designed to evaluate current HF management in 2013–2016 in a real-world setting [33]. The characteristics of the CHECK-HF registry have already been reported [33] but findings are still unpublished.
In summary, this survey study provides useful information regarding the opinion of cardiologists of different relevant aspects of the care of patients with HF attended in routine daily practice. The study highlights the importance of the patient’s education on knowledge of the disease and HF drugs, the need to have enough time during consultation for active assessment of adherence, in particular, in elderly patients, the relevant role of a good doctor-patient communication, and the usefulness of strategies of combining two or more active principles in a single pill. Actions suggested for improving treatment adherence included implementation of educational interventions and techniques for monitoring adherence, as well as empowerment of caregivers, development of patient expert programmes, potentiation of the role of well trained nurses and closed follow-up of patients by HF unit professionals.
Conflicts of interest:
Funding: The study was supported by Laboratorios SERVIER, S.L., Madrid, Spain. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgements
The authors thank Grupo Saned, S.L., for logistic support and Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.
References
Discussion
This study provides information on the opinion of cardiologists involved in the care of patients with HF regarding different aspects related to treatment adherence. Despite the decrease of cardiovascular mortality and the introduction of effective and safe medication treatments, HF continues to be a common cause of death and a leading disorder for the need of hospitalization and in-patient care [23]. Moreover, therapeutic recommendations developed in guidelines for the diagnosis and management of acute and chronic HF are applied to an unsatisfactory degree in daily practice [24]. There are multiple factors involved in suboptimal compliance with guidelines, including unawareness of the recommendations, poor acceptance due to discrepancies between guidelines in particular aspects, difficulties of implementation in routine practice related to local circumstances, equivocal assessment of the patient’s risk, or lack of coordination among the different specialists involved in the management of HF patients.
On the other hand, poor adherence has been consistently recognized as an important factor that compromises patient outcomes. Non-compliance is common in elderly patients with HF as were shortcomings in patients’ knowledge regarding prescribed medication, despite efforts to give adequate information [25]. In our study, 84% of participants considered that the patient’s age influences a lot or quite a lot on adherence to treatment. Likewise, it has been shown that forgetfulness, social support, and patient-provider relationship are related to adherence. Providers seeking to increase adherence must consider patients' expectations for their health, their environment, their barriers to following prescribed regimen, and their understanding of their condition and how it relates to medication prescribed [26]. In the present survey, patient’s knowledge of the disease and patient’s knowledge of the medicines prescribed were recognized as important influential factors related to adherence by 95.5% and 83.5% of cardiologists, respectively. In this respect, more than half of participants (57.6%) mentioned patient education as the first action to be implemented in their settings to improve adherence.
Also, good patient-doctor communication was reported as a very influential factor of adherent behaviour. It has been shown that patient-provider interactions appear to be a major determinant of medication adherence [27]. Providing tailored information, patient satisfaction with the communication received, and beliefs about medication are connected and can lead to improved medication adherence. Poor physician communication alone increases the risk of non-adherence. In a meta-analysis of 106 studies assessing the relationship between patient treatment adherence and physician-patient communication, there was a 19% higher risk of non-adherence among patients whose physician communicates poorly than among patients whose physician communicates well [28]. In addition, 95.5% of cardiologists considered that having available an established plan of prescribed medications is a very convenient or quite convenient as a practical tool to improve adherence. The provision of clear written instructions is a well-known method to improve adherence [29]. Mobile applications, automated check-ins, and text message medication reminders have been suggested as potential modes for improving adherence [30].
Some 80% of participants established criteria of active search of lack of adherence in their patients, with direct questioning at the patient interview in 82% of the cases. However, direct questioning may not provide accurate assessments, especially if closed-ended or judgmental questions are posed [31]. In the group of participants that did not use active criteria to examine medication adherence, lack of time was the main reason argued by 77% of participants. In this respect, there is a need for improvement establishing the adequate measures in the organization of the healthcare system at local levels, in order to allow sufficient time during routine consultations. Nurses have a key role in educational interventions, monitoring of decompensation signs, and improve treatment adherence especially in patients with HF followed by the nursing staff in specialized clinics.
Factors related to treatment that showed a higher impact on therapeutic decisions were, firstly, the aim of improving the prognosis of patients with HF and, secondly, the effect of treatment of amelioration of symptoms and improvements of the quality of life and functioning capacity of patients. Preferences of the patient, economic cost, conciliation with other drugs, safety or aspects favouring adherence were not rated as proprieties for treatment decisions, with percentages of participants selecting these reasons as first options ranging between 2% and 6%. In relation to diagnosis of HF, clinical criteria (Framingham) were stated as first or second option by 59% of participants. Echocardiogram was selected as first or second option by 57.1% of cardiologists. This would indicate the need and importance of clinical suspicion of HF before confirmation of diagnosis by echocardiography. In the present survey, questions regarding how patients with HF are managed, in particular, to assess details of their medical treatment were not included, so that whether prescription of recommended medications in daily practice differs from guidelines was not examined. Results of the Euro Heart Failure Survey have shown that the prescription of recommended medications including ACE inhibitors and beta-blockers remains limited and that the daily dosage remains low, particularly for beta-blockers [32]. Recently, a large-scale HF registry in the Netherlands, the CHECK-HF registry, which enrolled nearly 11,000 unselected patients with chronic HF treated in outpatient clinics was designed to evaluate current HF management in 2013–2016 in a real-world setting [33]. The characteristics of the CHECK-HF registry have already been reported [33] but findings are still unpublished.
In summary, this survey study provides useful information regarding the opinion of cardiologists of different relevant aspects of the care of patients with HF attended in routine daily practice. The study highlights the importance of the patient’s education on knowledge of the disease and HF drugs, the need to have enough time during consultation for active assessment of adherence, in particular, in elderly patients, the relevant role of a good doctor-patient communication, and the usefulness of strategies of combining two or more active principles in a single pill. Actions suggested for improving treatment adherence included implementation of educational interventions and techniques for monitoring adherence, as well as empowerment of caregivers, development of patient expert programmes, potentiation of the role of well trained nurses and closed follow-up of patients by HF unit professionals.
Conflicts of interest:
Funding: The study was supported by Laboratorios SERVIER, S.L., Madrid, Spain. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgements
The authors thank Grupo Saned, S.L., for logistic support and Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.
References
 Factors associated with therapeutic decisions taken by cardiologists in the care of patients with HF are shown in Figure 2. The most frequently selected factor affecting treatment decisions was “improves the prognosis of the patient” (this item was selected as first or second option by 80% of participants) followed by “repercussion on symptoms, quality of life and patient’s functioning capacity” (this item was selected as first or second option by 75% of participants). Only 6% of participants selected “aspects that favour adherence to treatment” as first or second option in their therapeutic decision. Regarding the percentage of HF patients receiving specific treatment in which medication should be changed because of side effects, 65.8% of participants reported medication changes in up to 25% of patients and 30.4% between 26 and 50%.
Figure 2. Distribution of the percentages of responses regarding factors that intervene in the therapeutic decisions in patients with heart failure (HF).
Factors associated with therapeutic decisions taken by cardiologists in the care of patients with HF are shown in Figure 2. The most frequently selected factor affecting treatment decisions was “improves the prognosis of the patient” (this item was selected as first or second option by 80% of participants) followed by “repercussion on symptoms, quality of life and patient’s functioning capacity” (this item was selected as first or second option by 75% of participants). Only 6% of participants selected “aspects that favour adherence to treatment” as first or second option in their therapeutic decision. Regarding the percentage of HF patients receiving specific treatment in which medication should be changed because of side effects, 65.8% of participants reported medication changes in up to 25% of patients and 30.4% between 26 and 50%.
Figure 2. Distribution of the percentages of responses regarding factors that intervene in the therapeutic decisions in patients with heart failure (HF).
 Adherence to treatment
Results of this section of the questionnaire are shown in Table 1. The participants of the study had a median of 518 patients assigned to their consultations. A total of 44.9% of cardiologists stated that between 26% and 50% of patients attended in the last week were diagnosed with HF. Also, 127 participants (80.4%) reported to establish active search criteria for adherence to treatment in their patients, using direct questioning in the majority of cases (81.9%). However, in the remaining 31 participants (19.6%) not assessing adherence to treatment, lack of time was the main reason argued by 77.4% of them.
Adherence to treatment
Results of this section of the questionnaire are shown in Table 1. The participants of the study had a median of 518 patients assigned to their consultations. A total of 44.9% of cardiologists stated that between 26% and 50% of patients attended in the last week were diagnosed with HF. Also, 127 participants (80.4%) reported to establish active search criteria for adherence to treatment in their patients, using direct questioning in the majority of cases (81.9%). However, in the remaining 31 participants (19.6%) not assessing adherence to treatment, lack of time was the main reason argued by 77.4% of them.
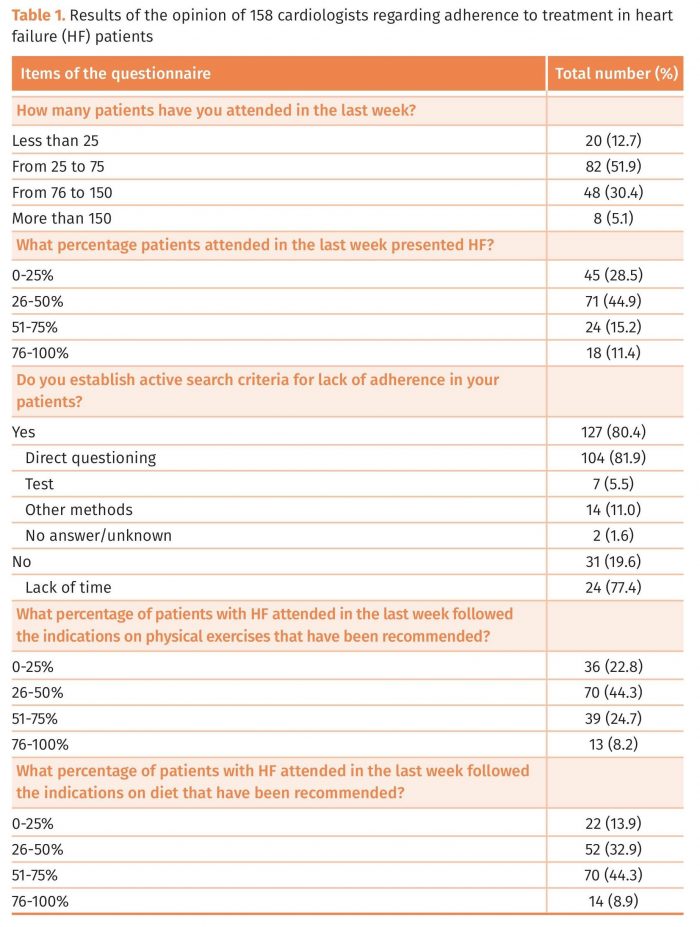 Overall, 67.1% of cardiologists recognized that less than 50% of patients followed recommendation on physical exercise. The percentages of participants who stated that between 0-25%, 26-50%, 51-75% and 76-100% of patients attended in the last week followed their recommendations were 22.8%, 44.3%, 24.7%, and 8.2%, respectively. On the other hand, between 51% and 75% of patients with HF attended in the last week followed recommendations on diet as stated by 44.3% of participants.
Non-modifiable factors associated with adherence to treatment
Results of this section of the questionnaire are shown in Table 2. Non-modifiable factors that were rated by participants as having “a lot” influence on adherence included to have an established plan of the prescribed medication (65.8% of respondents), patient’s education (69%), severity of illness perceived by the patient (49.4%), number of doses (45.6%), type of administration (31%), the age of the patient (30.4%), and interactions with other drugs (20.2%). However, almost all participants (98%) considered that the patient’s education influenced “a lot” or “quite a lot” in medication adherence, 95.5% that having available an established plan of prescribed medication influenced “a lot” or “quite a lot”, and 83.5% that the patient’s age influenced “a lot” or “quite a lot” in the adherence to treatment. Also, 91.8% of participants stated that in the chronic stage of the disease there was more risk for non-adherence to treatment.
Overall, 67.1% of cardiologists recognized that less than 50% of patients followed recommendation on physical exercise. The percentages of participants who stated that between 0-25%, 26-50%, 51-75% and 76-100% of patients attended in the last week followed their recommendations were 22.8%, 44.3%, 24.7%, and 8.2%, respectively. On the other hand, between 51% and 75% of patients with HF attended in the last week followed recommendations on diet as stated by 44.3% of participants.
Non-modifiable factors associated with adherence to treatment
Results of this section of the questionnaire are shown in Table 2. Non-modifiable factors that were rated by participants as having “a lot” influence on adherence included to have an established plan of the prescribed medication (65.8% of respondents), patient’s education (69%), severity of illness perceived by the patient (49.4%), number of doses (45.6%), type of administration (31%), the age of the patient (30.4%), and interactions with other drugs (20.2%). However, almost all participants (98%) considered that the patient’s education influenced “a lot” or “quite a lot” in medication adherence, 95.5% that having available an established plan of prescribed medication influenced “a lot” or “quite a lot”, and 83.5% that the patient’s age influenced “a lot” or “quite a lot” in the adherence to treatment. Also, 91.8% of participants stated that in the chronic stage of the disease there was more risk for non-adherence to treatment.
 Modifiable factors associated with adherence to treatment
A large majority of participants (90.5%) completely agree (50%) or quite agree (40.5%) that strategies directed to improve adherence should be established at individual level rather than collectively. As shown in Table 3, items that were considered “very influential” regarding adherence to treatment were a good doctor-patient relationship (stated by 82.3% of participants) and patient’s knowledge of his/her disease (stated by 70.2% of participants). The lack of coordination between different healthcare levels was reported as very influential on adherence by 51.3% of cardiologists. Other modifiable factors that may improve adherence “a lot” were family and social support (stated by 67.1% of participants), strategies based on joining two or more active principles in a single pill (stated by 69.6% of participants), and to have available an established plan of medicines prescribed for the treatment of HF (stated by 53.8% of participants). Specific intervention strategies to improve adherence and patient’s knowledge of the characteristics of their medications were also considered to have “a lot” of influence by 42.4% and 35.4% of participants, respectively.
Modifiable factors associated with adherence to treatment
A large majority of participants (90.5%) completely agree (50%) or quite agree (40.5%) that strategies directed to improve adherence should be established at individual level rather than collectively. As shown in Table 3, items that were considered “very influential” regarding adherence to treatment were a good doctor-patient relationship (stated by 82.3% of participants) and patient’s knowledge of his/her disease (stated by 70.2% of participants). The lack of coordination between different healthcare levels was reported as very influential on adherence by 51.3% of cardiologists. Other modifiable factors that may improve adherence “a lot” were family and social support (stated by 67.1% of participants), strategies based on joining two or more active principles in a single pill (stated by 69.6% of participants), and to have available an established plan of medicines prescribed for the treatment of HF (stated by 53.8% of participants). Specific intervention strategies to improve adherence and patient’s knowledge of the characteristics of their medications were also considered to have “a lot” of influence by 42.4% and 35.4% of participants, respectively.
 A total of 93.7% of participants considered that empowerment of caregivers could facilitate “a lot” or “quite a lot” therapeutic adherence. Also, 91.8% of participants believed that expert patient programmes could notably improve adherence (Figure 3). In relation to the open question of actions that may be perform in the cardiologist’s setting to improve adherence are summarized in Table 4, being, patient education-related interventions, involvement of training nurses and coordination of healthcare groups the most frequently stated.
Figure 3. Actions to improve adherence to treatment in heart failure. Percentages of response of participants according to influence on adherence.
A total of 93.7% of participants considered that empowerment of caregivers could facilitate “a lot” or “quite a lot” therapeutic adherence. Also, 91.8% of participants believed that expert patient programmes could notably improve adherence (Figure 3). In relation to the open question of actions that may be perform in the cardiologist’s setting to improve adherence are summarized in Table 4, being, patient education-related interventions, involvement of training nurses and coordination of healthcare groups the most frequently stated.
Figure 3. Actions to improve adherence to treatment in heart failure. Percentages of response of participants according to influence on adherence.
 Discussion
This study provides information on the opinion of cardiologists involved in the care of patients with HF regarding different aspects related to treatment adherence. Despite the decrease of cardiovascular mortality and the introduction of effective and safe medication treatments, HF continues to be a common cause of death and a leading disorder for the need of hospitalization and in-patient care [23]. Moreover, therapeutic recommendations developed in guidelines for the diagnosis and management of acute and chronic HF are applied to an unsatisfactory degree in daily practice [24]. There are multiple factors involved in suboptimal compliance with guidelines, including unawareness of the recommendations, poor acceptance due to discrepancies between guidelines in particular aspects, difficulties of implementation in routine practice related to local circumstances, equivocal assessment of the patient’s risk, or lack of coordination among the different specialists involved in the management of HF patients.
On the other hand, poor adherence has been consistently recognized as an important factor that compromises patient outcomes. Non-compliance is common in elderly patients with HF as were shortcomings in patients’ knowledge regarding prescribed medication, despite efforts to give adequate information [25]. In our study, 84% of participants considered that the patient’s age influences a lot or quite a lot on adherence to treatment. Likewise, it has been shown that forgetfulness, social support, and patient-provider relationship are related to adherence. Providers seeking to increase adherence must consider patients' expectations for their health, their environment, their barriers to following prescribed regimen, and their understanding of their condition and how it relates to medication prescribed [26]. In the present survey, patient’s knowledge of the disease and patient’s knowledge of the medicines prescribed were recognized as important influential factors related to adherence by 95.5% and 83.5% of cardiologists, respectively. In this respect, more than half of participants (57.6%) mentioned patient education as the first action to be implemented in their settings to improve adherence.
Also, good patient-doctor communication was reported as a very influential factor of adherent behaviour. It has been shown that patient-provider interactions appear to be a major determinant of medication adherence [27]. Providing tailored information, patient satisfaction with the communication received, and beliefs about medication are connected and can lead to improved medication adherence. Poor physician communication alone increases the risk of non-adherence. In a meta-analysis of 106 studies assessing the relationship between patient treatment adherence and physician-patient communication, there was a 19% higher risk of non-adherence among patients whose physician communicates poorly than among patients whose physician communicates well [28]. In addition, 95.5% of cardiologists considered that having available an established plan of prescribed medications is a very convenient or quite convenient as a practical tool to improve adherence. The provision of clear written instructions is a well-known method to improve adherence [29]. Mobile applications, automated check-ins, and text message medication reminders have been suggested as potential modes for improving adherence [30].
Some 80% of participants established criteria of active search of lack of adherence in their patients, with direct questioning at the patient interview in 82% of the cases. However, direct questioning may not provide accurate assessments, especially if closed-ended or judgmental questions are posed [31]. In the group of participants that did not use active criteria to examine medication adherence, lack of time was the main reason argued by 77% of participants. In this respect, there is a need for improvement establishing the adequate measures in the organization of the healthcare system at local levels, in order to allow sufficient time during routine consultations. Nurses have a key role in educational interventions, monitoring of decompensation signs, and improve treatment adherence especially in patients with HF followed by the nursing staff in specialized clinics.
Factors related to treatment that showed a higher impact on therapeutic decisions were, firstly, the aim of improving the prognosis of patients with HF and, secondly, the effect of treatment of amelioration of symptoms and improvements of the quality of life and functioning capacity of patients. Preferences of the patient, economic cost, conciliation with other drugs, safety or aspects favouring adherence were not rated as proprieties for treatment decisions, with percentages of participants selecting these reasons as first options ranging between 2% and 6%. In relation to diagnosis of HF, clinical criteria (Framingham) were stated as first or second option by 59% of participants. Echocardiogram was selected as first or second option by 57.1% of cardiologists. This would indicate the need and importance of clinical suspicion of HF before confirmation of diagnosis by echocardiography. In the present survey, questions regarding how patients with HF are managed, in particular, to assess details of their medical treatment were not included, so that whether prescription of recommended medications in daily practice differs from guidelines was not examined. Results of the Euro Heart Failure Survey have shown that the prescription of recommended medications including ACE inhibitors and beta-blockers remains limited and that the daily dosage remains low, particularly for beta-blockers [32]. Recently, a large-scale HF registry in the Netherlands, the CHECK-HF registry, which enrolled nearly 11,000 unselected patients with chronic HF treated in outpatient clinics was designed to evaluate current HF management in 2013–2016 in a real-world setting [33]. The characteristics of the CHECK-HF registry have already been reported [33] but findings are still unpublished.
In summary, this survey study provides useful information regarding the opinion of cardiologists of different relevant aspects of the care of patients with HF attended in routine daily practice. The study highlights the importance of the patient’s education on knowledge of the disease and HF drugs, the need to have enough time during consultation for active assessment of adherence, in particular, in elderly patients, the relevant role of a good doctor-patient communication, and the usefulness of strategies of combining two or more active principles in a single pill. Actions suggested for improving treatment adherence included implementation of educational interventions and techniques for monitoring adherence, as well as empowerment of caregivers, development of patient expert programmes, potentiation of the role of well trained nurses and closed follow-up of patients by HF unit professionals.
Conflicts of interest:
Funding: The study was supported by Laboratorios SERVIER, S.L., Madrid, Spain. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgements
The authors thank Grupo Saned, S.L., for logistic support and Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.
References
Discussion
This study provides information on the opinion of cardiologists involved in the care of patients with HF regarding different aspects related to treatment adherence. Despite the decrease of cardiovascular mortality and the introduction of effective and safe medication treatments, HF continues to be a common cause of death and a leading disorder for the need of hospitalization and in-patient care [23]. Moreover, therapeutic recommendations developed in guidelines for the diagnosis and management of acute and chronic HF are applied to an unsatisfactory degree in daily practice [24]. There are multiple factors involved in suboptimal compliance with guidelines, including unawareness of the recommendations, poor acceptance due to discrepancies between guidelines in particular aspects, difficulties of implementation in routine practice related to local circumstances, equivocal assessment of the patient’s risk, or lack of coordination among the different specialists involved in the management of HF patients.
On the other hand, poor adherence has been consistently recognized as an important factor that compromises patient outcomes. Non-compliance is common in elderly patients with HF as were shortcomings in patients’ knowledge regarding prescribed medication, despite efforts to give adequate information [25]. In our study, 84% of participants considered that the patient’s age influences a lot or quite a lot on adherence to treatment. Likewise, it has been shown that forgetfulness, social support, and patient-provider relationship are related to adherence. Providers seeking to increase adherence must consider patients' expectations for their health, their environment, their barriers to following prescribed regimen, and their understanding of their condition and how it relates to medication prescribed [26]. In the present survey, patient’s knowledge of the disease and patient’s knowledge of the medicines prescribed were recognized as important influential factors related to adherence by 95.5% and 83.5% of cardiologists, respectively. In this respect, more than half of participants (57.6%) mentioned patient education as the first action to be implemented in their settings to improve adherence.
Also, good patient-doctor communication was reported as a very influential factor of adherent behaviour. It has been shown that patient-provider interactions appear to be a major determinant of medication adherence [27]. Providing tailored information, patient satisfaction with the communication received, and beliefs about medication are connected and can lead to improved medication adherence. Poor physician communication alone increases the risk of non-adherence. In a meta-analysis of 106 studies assessing the relationship between patient treatment adherence and physician-patient communication, there was a 19% higher risk of non-adherence among patients whose physician communicates poorly than among patients whose physician communicates well [28]. In addition, 95.5% of cardiologists considered that having available an established plan of prescribed medications is a very convenient or quite convenient as a practical tool to improve adherence. The provision of clear written instructions is a well-known method to improve adherence [29]. Mobile applications, automated check-ins, and text message medication reminders have been suggested as potential modes for improving adherence [30].
Some 80% of participants established criteria of active search of lack of adherence in their patients, with direct questioning at the patient interview in 82% of the cases. However, direct questioning may not provide accurate assessments, especially if closed-ended or judgmental questions are posed [31]. In the group of participants that did not use active criteria to examine medication adherence, lack of time was the main reason argued by 77% of participants. In this respect, there is a need for improvement establishing the adequate measures in the organization of the healthcare system at local levels, in order to allow sufficient time during routine consultations. Nurses have a key role in educational interventions, monitoring of decompensation signs, and improve treatment adherence especially in patients with HF followed by the nursing staff in specialized clinics.
Factors related to treatment that showed a higher impact on therapeutic decisions were, firstly, the aim of improving the prognosis of patients with HF and, secondly, the effect of treatment of amelioration of symptoms and improvements of the quality of life and functioning capacity of patients. Preferences of the patient, economic cost, conciliation with other drugs, safety or aspects favouring adherence were not rated as proprieties for treatment decisions, with percentages of participants selecting these reasons as first options ranging between 2% and 6%. In relation to diagnosis of HF, clinical criteria (Framingham) were stated as first or second option by 59% of participants. Echocardiogram was selected as first or second option by 57.1% of cardiologists. This would indicate the need and importance of clinical suspicion of HF before confirmation of diagnosis by echocardiography. In the present survey, questions regarding how patients with HF are managed, in particular, to assess details of their medical treatment were not included, so that whether prescription of recommended medications in daily practice differs from guidelines was not examined. Results of the Euro Heart Failure Survey have shown that the prescription of recommended medications including ACE inhibitors and beta-blockers remains limited and that the daily dosage remains low, particularly for beta-blockers [32]. Recently, a large-scale HF registry in the Netherlands, the CHECK-HF registry, which enrolled nearly 11,000 unselected patients with chronic HF treated in outpatient clinics was designed to evaluate current HF management in 2013–2016 in a real-world setting [33]. The characteristics of the CHECK-HF registry have already been reported [33] but findings are still unpublished.
In summary, this survey study provides useful information regarding the opinion of cardiologists of different relevant aspects of the care of patients with HF attended in routine daily practice. The study highlights the importance of the patient’s education on knowledge of the disease and HF drugs, the need to have enough time during consultation for active assessment of adherence, in particular, in elderly patients, the relevant role of a good doctor-patient communication, and the usefulness of strategies of combining two or more active principles in a single pill. Actions suggested for improving treatment adherence included implementation of educational interventions and techniques for monitoring adherence, as well as empowerment of caregivers, development of patient expert programmes, potentiation of the role of well trained nurses and closed follow-up of patients by HF unit professionals.
Conflicts of interest:
Funding: The study was supported by Laboratorios SERVIER, S.L., Madrid, Spain. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgements
The authors thank Grupo Saned, S.L., for logistic support and Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.
References
- Cowie MR, Lopatin YM, Saldarriaga C, Fonseca C, Sim D, Magaña JA, Albuquerque D, Trivi M, Moncada G, González Castillo BA, Sánchez MOS, Chung E. The Optimize Heart Failure Care Program: initial lessons from global implementation. Int J Cardiol 2017; 236: 340-344.
- Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CSP, Sato N, Shah AN, Gheorghiade M. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 2014; 63: 1123-1133.
- Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, Allison M, Hemingway H, Cleland JG, McMurray JJV, Rahimi K. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. Lancet 2018; 391: 572-580.
- von Lueder TG, Agewall S. The burden of heart failure in the general population: a clearer and more concerning picture. J Thorac Dis 2018; 10(Suppl 17): S1934-S1937.
- Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, Killian JM, Roger VL. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Intern Med 2015; 175: 996-1004.
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017; 135: e146-e603.
- Fonarow GC, Abraham WT, Albert NM, Stough WG, Gheorghiade M, Greenberg BH, O'Connor CM, Pieper K, Sun JL, Yancy CW, Young JB; OPTIMIZE-HF Investigators and Hospitals. Factors identified as precipitating hospital admissions for heart failure and clinical outcomes: findings from OPTIMIZE-HF. Arch Intern Med 2008; 168: 847-854.
- Farmakis D, Parissis J, Lekakis J, Filippatos G. Acute heart failure: epidemiology, risk factors, and prevention. Rev Esp Cardiol (Engl Ed) 2015; 68: 245-248.
- Hood SR, Giazzon AJ, Seamon G, Lane KA, Wang J, Eckert GJ, Tu W, Murray MD. Association between medication adherence and the outcomes of heart failure. Pharmacotherapy 2018; 38: 539-545.
- Ruppar TM, Delgado JM, Temple J. Medication adherence interventions for heart failure patients: a meta-analysis. Eur J Cardiovasc Nurs 2015; 14: 395-404.
- Reed BN, Rodgers JE, Sueta CA. Polypharmacy in heart failure: drugs to use and avoid. Heart Failure Clin 2014; 10: 577-590.
- Allen LA, Fonarow GC, Liang L, Schulte PJ, Masoudi FA, Rumsfeld JS, Ho PM, Eapen ZJ, Hernandez AF, Heidenreich PA, Bhatt DL, Peterson ED, Krumholz HM. Medication initiation burden required to comply with heart failure guideline recommendations and hospital quality measures. Circulation 2015; 132: 1347–1353.
- Shah D, Simms K, Barksdale DJ, Wu JR. Improving medication adherence of patients with chronic heart failure: challenges and solutions. Res Rep Clin Cardiol 2015; 6: 87-95.
- Lee D, Mansi I, Bushuan S, Parish R. Non-adherence in at-risk heart failure patients: characteristics and outcomes. J Nat Sci 2015; 1: Available from: http://www.jnsci.org/content/95. Accessed November 15, 2018.
- Corrao G, Rea F, Ghirardi A, Soranna D, Merlino L, Mancia G. Adherence with antihypertensive drug therapy and the risk of heart failure in clinical practice. Hypertension 2015; 66: 742-749.
- Ruppar TM, Cooper PS, Mehr DR, Delgado JM, Dunbar-Jacob JM. Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials. J Am Heart Assoc 2016; 5. pii: e002606. doi: 10.1161/JAHA.115.002606.
- Shanbhag D, Graham ID, Harlos K, Haynes RB, Gabizon I, Connolly SJ, Van Spall HGC. Effectiveness of implementation interventions in improving physician adherence to guideline recommendations in heart failure: a systematic review. BMJ Open 2018; 8: doi: 10.1136/bmjopen-2017-017765.
- Giezeman M, Arne M, Theander K. Adherence to guidelines in patients with chronic heart failure in primary health care. Scand J Prim Health Care 2017; 35: 336-343.
- Komajda M, Cowie MR, Tavazzi L, Ponikowski P, Anker SD, Filippatos GS; QUALIFY Investigators. Physicians' guideline adherence is associated with better prognosis in outpatients with heart failure with reduced ejection fraction: the QUALIFY international registry. Eur J Heart Fail 2017; 19: 1414-1423.
- Remme WJ, McMurray JJ, Hobbs FD, Cohen-Solal A, Lopez-Sendon J, Boccanelli A, Zannad F, Rauch B, Keukelaar K, Macarie C, Ruzyllo W, Cline C; SHAPE Study Group. Awareness and perception of heart failure among European cardiologists, internists, geriatricians, and primary care physicians. Eur Heart J 2008; 29: 1739-1752.
- Salvador MJ, Sebaoun A, Sonntag F, Blanch P, Silber S, Aznar J, Komajda M; Council for Cardiology Practice de la Sociedad Europea de Cardiologia. European study of ambulatory management of heart failure by cardiologists. Rev Esp Cardiol 2004; 57: 1170-1178.
- Crespo Leiro MG, Matalí A, López-Sendñon JL. Medication adherence in patients with heart failure and a depressed ejection fraction attending cardiology clinics. Rev Esp Cardiol 2009; 62: 454-455.
- Unverzagt S, Meyer G, Mittmann S, Samos FA, Unverzagt M, Prondzinsky R. Improving Treatment Adherence in Heart Failure. Dtsch Arztebl Int 2016; 113: 423-430.
- López-Sendón J, López de Sá E. Poblems in the application of clinical practice guidelines in postinfarction heart failure. [Article in Spanish]. Rev Esp Cardiol 2006; 6: 59B-68B.
- Cline CM1, Björck-Linné AK, Israelsson BY, Willenheimer RB, Erhardt LR. Non-compliance and knowledge of prescribed medication in elderly patients with heart failure. Eur J Heart Failure 1999; 1: 145-149.
- Wu JR, Moser DK, Lennie TA, Burkhart PV. Medication adherence in patients who have heart failure: a review of the literature. Nurs Clin North Am 2008; 43: 133-153.
- Zullig LL, Shaw RJ, Shah BR, Peterson ED, Lindquist JH, Crowley MJ, Grambow SC, Bosworth HB. Patient-provider communication, self-reported medication adherence, and race in a postmyocardial infarction population. Patient Prefer Adherence. 2015; 9: 311-318.
- Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care 2009; 47: 826-834.
- Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J 2011; 26: 155-159.
- Aggarwal B, Pender A, Mosca L, Mochari-Greenberger H. Factors associated with medication adherence among heart failure patients and their caregivers. J Nurs Educ Pract 2015; 5: 22-27.
- MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging 2005; 22: 231-235.
- Komajda M, Follath F, Swedberg K, Cleland J, Aguilar JC, Cohen-Solal A, Dietz R, Gavazzi A, Van Gilst WH, Hobbs R, Korewicki J, Madeira HC, Moiseyev VS, Preda I, Widimsky J, Freemantle N, Eastaugh J, Mason J; Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology. The EuroHeart Failure Survey programme--a survey on the quality of care among patients with heart failure in Europe. Part 2: treatment. Eur Heart J 2003; 24: 464-474.
- Brugts JJ, Linssen GCM, Hoes AW, Brunner-La Rocca HP; CHECK-HF investigators. Real-world heart failure management in 10,910 patients with chronic heart failure in the Netherlands : design and rationale of the Chronic Heart failure ESC guideline-based Cardiology practice Quality project (CHECK-HF) registry. Neth Heart J 2018; 26: 272-279.


